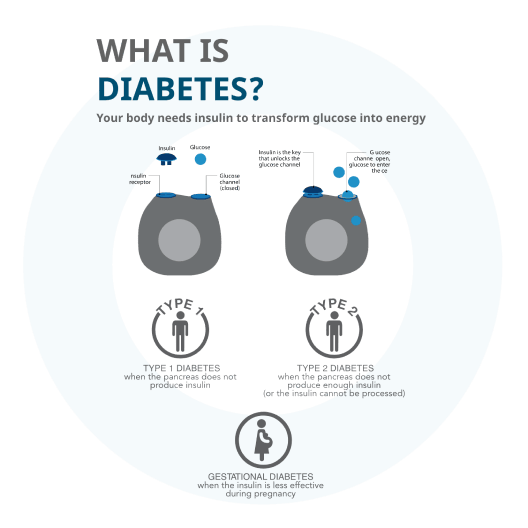
Gestational diabetes
Gestational diabetes (GDM) is a form of diabetes consisting of high blood glucose levels during pregnancy. It develops in one in 25 pregnancies worldwide and is associated with complications to both mother and baby. GDM usually disappears after pregnancy but women with GDM and their children are at an increased risk of developing type 2 diabetes later in life. Approximately half of women with a history of GDM go on to develop type 2 diabetes within five to ten years after delivery.
Understanding your diagnosis of gestational diabetes
If you are diagnosed with gestational diabetes, it is important to take the right steps toward controlling the level of blood glucose in the body. If left undetected or not correctly controlled, it will increase the risk of the following:
- If your blood glucose is too high, your baby will produce more insulin, which can make your baby grow bigger, thereby increasing the likelihood of having your labour induced or undergoing a caesarean section.
- High maternal blood glucose can lead to serious birth problems and stillbirth
- The baby could develop hypoglycaemia, respiratory distress, and jaundice
- The baby may develop a calcium and magnesium deficiency. The good news is that the majority of gestational diabetes cases are easily managed with diet and lifestyle measures such as exercise.
However, if these measures are not enough to keep the all-important blood sugars in control, then medication or even insulin injections may be required. Your doctor will be able to guide you through what is best for you once you have been diagnosed and the best treatment plan to follow in terms of diet, exercise or possible medication.
Tips for coping with gestational diabetes during pregnancy
As always, it is best to refer to a dietician to create a meal plan based on your weight, pregnancy weight gain goals, blood sugar levels and levels of activity, but in general a balance of carbohydrates, nutritious meals and staying in control of the timing and portion size of meals are a good start.

Medication
If you have been taking medication prior to being diagnosed with gestational diabetes, check with your doctor whether it is still safe to do so. For example, patients are asked to stop taking cholesterol lowering medication and some blood pressure medications during pregnancy
Pregnancy when you already have type 1 or type 2 diabetes
Women diagnosed with either of these types of diabetes can have healthy pregnancies, but they need to take extra care of themselves, ensuring a good diet and regular monitoring of blood glucose levels.
Women with type 1 and 2 diabetes can have a healthy pregnancy if blood glucose levels are controlled before and throughout the pregnancy. That begins with monitoring her blood glucose levels if she is planning to have a baby as well as having good control over her blood glucose levels prior to pregnancy.
If high blood sugar (hyperglycaemia) is present in the first eight weeks of pregnancy, the foetus is at risk of birth defects. In the later stages of pregnancy, if the hyperglycaemia persists that may result in a larger baby, leading to delivery complications and increasing the risk for a caesarean section.
Care during pregnancy
- Women with type 1 and 2 diabetes should regularly have their eyes checked by a specialist as they are at a higher risk for developing retinopathy (damage to vessels of the eye) during pregnancy.
- Changes to the kidneys may also occur in a small percentage of women if damage was already present prior to pregnancy. To monitor the function of the kidneys, blood work should be done for regular check-ups.
- Certain blood pressure medications (ARBs and ACEs) and cholesterol lowering statins are not recommended during pregnancy. Speak to your doctor about alternatives to these medications when pregnant.
- Insulin resistance increases throughout pregnancy, but usually starts around 14 weeks. Most women with type 2 diabetes who are on oral hypoglycaemic agents (OHAs) will be changed to insulin to optimise blood glucose control.
- Folic acid is a man-made form of Vitamin B called folate that plays an important role in the production of red blood cells and helps your baby’s neural tube develop into their brain and spinal cord. The recommendation for women planning a pregnancy is to take 5mg of folic acid three months prior to conception until three months post conception.
Determining insulin needs
Insulin needs change throughout pregnancy. Blood glucose levels may be variable in the first trimester due to insulin sensitivity, nausea and vomiting. It is recommended to eat three meals and snacks as needed (at least one at bedtime), which can help with managing your blood glucose levels and determining your insulin needs.
Blood glucose targets
For women with gestational diabetes or pre-existing type 1 or type 2 diabetes in pregnancy, the following targets are recommended:
- Fasting: less than 95 mg/dL (5.3 mmol/L) and either
- One-hour after meals: less than 140 mg/dL (7.8 mmol/L) or
- Two-hour after meals: less than 120 mg/dL (6.7 mmol/L)
Regular activity is beneficial to keep good control of blood glucose levels, manage weight gain and increase energy levels. Speak with your doctor if there may be activity limitations.
Low blood sugar (hypoglycaemia) occurs when the level of glucose in your blood drops to levels that are considered to be below normal